Resource for healthcare providers
It is important to consider how treatment decisions align with a patient’s wishes, values, and beliefs for their care. In Ontario, Advance Care Planning, Goals of Care, and Treatment Decisions & Informed Consent are situated along a Person-Centred Decision-Making continuum, as pictured in the diagram below.
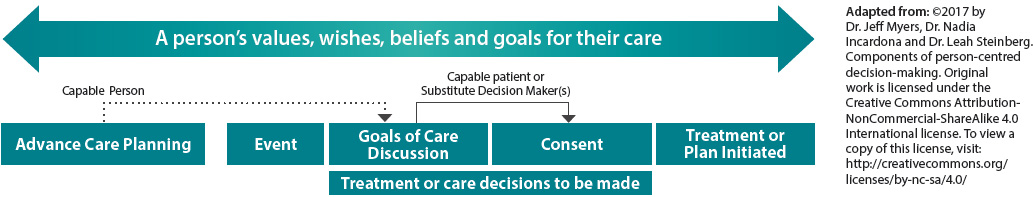
Goals of Care (GOC) Conversations
Current care
Discussions between a provider and a capable patient (or the incapable patient’s Substitute Decision Maker [SDM]) that focus on:
- Ensuring the patient understands the serious (and/or sometimes incurable and progressive) nature of their illness, and
- Helping the healthcare provider to understand the patient’s
values and the goals they have for their care.
The discussion is focused on the current clinical context. Outcome: Patient and healthcare providers have a shared understanding of the patient’s goals for their care. These goals arethen used to support treatment decisions and informed consent.
How do I have a GOC conversation?*
1. Explore Illness understanding: Check the patient’s understanding of their diagnosis and prognosis. Confirm their understanding of their illness.
2. Inform: Clarify the patient/family’s interest in knowing more about their illness and the prognosis. Provide information. Allow questions and resolve outstanding concerns.
3. Elicit values and define goals:
- Explore the patient’s past experiences, hopes, values
and priorities; - Discuss the patient’s perception of quality of life and what they consider important; and
- Ask the patient to describe the goals they have for their care and help them to define the meaning of these goals.
4. Plan and Document: Document the identified GOC. Use these goals to inform the development of a Plan of Treatment with the patient. Provide copies of documentation to the patient and/or their SDM.
5. Revisit: Revisit this discussion regularly, especially if the
patient’s health status changes. Update the GOC and Plan
of Treatment accordingly.
Advance Care Planning (ACP) Conversations
Future care
ACP involves the patient (while capable):
- Confirming their future Substitute Decision Maker by accepting the automatic SDM or assigning a Power of Attorney for Personal Care (POAPC), and
- Discussing their wishes, values, and beliefs with their SDM.
Outcome: Patient has shared their wishes and values with their
SDM to prepare their SDM for future decision-making.
Treatment Decisions & Informed Consent
Current treatment
Informed and contextualized treatment decisions are made by the patient (or their Substitute Decision Maker if incapable).
Consent requires providing the patient with information about the nature of treatment, benefits, risks, side effects, alternative courses of action, and likely consequences of not receiving treatment.
The conversation is focused on the current clinical (treatment oriented) context.
Outcome: Informed consent to treatment(s) (e.g. code status)
For more tips on how to facilitate Goals of Care conversations with a patient (or SDM), please see: Approaches to Goals of Care Conversations: Resource for healthcare providers
* Adapted from Goals of Care ELearning Module created by Leah Steinberg and Christine Soong, Sinai Health System